How To Tell If Someone Has an STD
It’s often said that appearances can be deceiving, akin to mistaking a calm sea for the absence of turbulent currents below.
Hidden symptoms of STDs often lurk unseen, like a silent predator awaiting its unwary prey – a stark reminder of the intricacies beneath the surface.
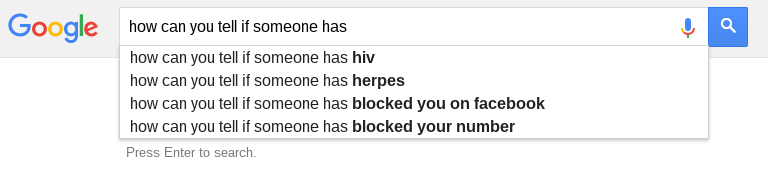
How Can You Tell If Someone Has An STD?
Recognizing STD Symptoms
Getting tested for STDs is the only way to know with 100 percent certainty whether someone has an STD. However, there are certain signs and symptoms that can be useful if you’re worried about how to tell if someone has an STD. Subtle physical manifestations can hint at an underlying STD, including unusual genital discharge, persistent itching, or aberrant bleeding, which should never be dismissed. Pain during urination or sexual intercourse may also be a telltale sign of an infection that requires immediate attention.
Such symptoms demand a higher degree of vigilance, particularly if they emerge following a new sexual encounter. Prompt medical consultation can elucidate the nature of these symptoms and guide appropriate interventions.
Questions to ask yourself to help gauge if they have an STD:
Does this person have bumps on their genitals or mouth?
- Bumps, warts, pimples, blisters, or sores on or around the genitals can be caused by:
- HSV-1, known as oral herpes, and HSV-2, known as genital herpes: Lesions
- Molluscum contagiosum: Flesh-toned spots with a sunken, concave appearance
- HPV: Genital warts
- Scabs on or around the genitals are typically a sign of bumps that have oozed and started healing
Does this person have a sore throat or throat infection? It could be a sign of:
- Sore throat, difficulty swallowing, redness, pockets of pus, chancre sores in the mouth or on the throat, loss of voice, and (in rare cases) throat fungus can be caused by:
- Chlamydia
- Gonorrhea: Swollen glands in the throat
- Syphilis: Large, gray or white lesions
- HIV: White or yellowish fungal infection
- HPV
Does this person have chronic flu-like symptoms?
- Fever, chills, fatigue, swollen joints, and nausea can all be signs of an STD, such as:
- HIV
- Chlamydia
- Gonorrhea
- Syphilis
Does this person have a rash?
- Rash on the palms of the hands or soles of the feet can be caused by:
- Secondary stage syphilis: Red or brown, non itchy rash
Does this person have pink eye?
- Conjunctivitis, known as pink eye, can be caused by:
- Gonorrhea
- Chlamydia
- Herpes
Does this person have encephalitis or meningitis?
- Lymphocytic Meningitis (Mollaret’s meningitis), a disease caused by swelling of the protective membranes of the brain and spinal cord, can be caused by:
- Herpes simplex 1 (HSV-1), the virus that most commonly causes oral herpes
Does this person have a high-risk job?
- Certain jobs carry a higher risk of contracting an STD, such as:
- Obstetricians and gynecologists (OB/GYNs)
- Physicians, nurses, EMTs, first responders, and other hospital staff
- Aid workers/Missionaries
- Janitorial staff who work with bodily waste or contaminated water
- Sex workers and adult entertainers
There are many other possible indicators that someone has an STD, but without an STD test, there is no way to be absolutely sure. What may look like a bump on the penis could be an ingrown hair. It can be difficult to distinguish between normal and abnormal vaginal discharge. Burning or itching during urination could be due to a urinary tract infection and itching in the genital area could be a result of an allergic reaction to a new laundry detergent. Conversely, something that seems completely non-sexual, like a rash on your armpit or spotting between menstrual cycles, could be the first sign of an infection that if unnoticed and untreated, could lead to very serious side effects. The best way to avoid STDs if you are sexually active is to practice safe sex and get tested regularly.
Additionally here are some signs to look out for if you think someone might have an STD.
A Deeper Look at Visual STD Symptoms
Skin Manifestations: Bumps and Rashes
Bumps and rashes can be pivotal indicators of underlying sexually transmitted infections (STIs).
Syphilis often presents a non-itchy rash on palms and soles, indicative of its systemic impact beyond genital regions.
Identification of unusual lesions or rashes necessitates professional evaluation, as self-diagnosis can lead to misinterpretation and delayed treatment. Early intervention can mitigate complications, highlighting the importance of recognizing skin changes as potential harbingers of STIs.
Discomforts: Sore Throats and Joint Pain
A sore throat can often be, misleadingly, attributed to non-sexual illnesses.
However, when considering the constellation of potential STD symptoms, a persistent sore throat warrants a more in-depth investigation, particularly when it coexists with other suggestive signs, such as lesions or pain during swallowing. A healthcare provider can discern whether it’s an STD-related symptom or a result of common respiratory infections.
Systemic manifestations, including joint pain, may accompany STDs like gonorrhea and chlamydia, though they more commonly connote diseases like Lyme or rheumatoid arthritis. Specialized testing can unravel the true source of discomfort, ensuring appropriate management and relief.
For instance, syphilis and gonorrhea can trigger widespread inflammation, reflecting their ability to affect multiple organ systems. Recognizing these symptoms as potential STD indicators is crucial for timely diagnosis and treatment before long-term consequences develop.
While these could easily be dismissed as unrelated to sexual health, they often require a comprehensive medical evaluation to rule out STDs. Addressing these discomforts promptly can not only provide relief but also prevent the transmission of the disorder and protect against serious health complications.
Unusual Discharges: When to Worry
Vaginal or penile discharges can signal an STD when they deviate from the norm in color, consistency, or smell.
- Yellow or green discharge could indicate gonorrhea or trichomoniasis.
- Thick, white, and clumpy discharge, resembling cottage cheese, is often a sign of a yeast infection but can also suggest gonorrhea in some cases.
- Foul-smelling discharge, especially when accompanied by pain, may be symptomatic of bacterial vaginosis or trichomoniasis.
- Bloody or brown discharge outside of menstrual periods could be a warning for chlamydia, gonorrhea, or vaginal atrophy.It’s essential to get evaluated by a healthcare professional if you observe such changes.
Delayed diagnosis puts you at risk for complications and increases the likelihood of transmitting the infection to others.
Assessing Behavioral Risk Factors
While physical manifestations provide vital clues, an individual’s history and behaviors are equally critical. Engaging in unprotected intercourse, having multiple sexual partners, or a known exposure to sexually transmitted infections elevates risk markedly. Past diagnosis of an STD implies a greater likelihood of a current one, emphasizing the importance of candid dialogue and regular screenings to manage and mitigate potential risks.
Sexual History: A Candid Conversation
Discourse on prior sexual encounters is crucial, offering insights that transcend the physical evidence of infection. Open and honest discussions about sexual history can significantly augment the risk assessment process and facilitate early detection and treatment of STDs.
The intricacy of such dialogue necessitates a respectful and non-judgmental approach, ensuring that partners feel secure sharing their history. Questions regarding previous diagnoses, number of partners, types of sexual activities engaged in, and the consistent use of protection are pertinent. This transparency not only fosters trust but can directly impact the health and safety of all individuals involved.
Moreover, a comprehensive sexual history should incorporate inquiries about any known risk behaviors or exposures. This dialogue can reveal a history of substance use that may influence unsafe sexual practices, or encounters with partners whose STD status is unknown or positive. Understanding these factors is imperative for creating a complete risk profile.
Ultimately, the goal is an open exchange that leads to proactive health decisions. It encourages partners to seek testing and preventative measures, like HPV vaccination or regular STD screenings, reinforcing the notion that sexual health is a shared responsibility. Such discussions can dispel myths, alleviate stigma, and ensure individuals are equipped to make informed choices about their sexual wellbeing.
High-Risk Professions: Understanding the Exposure
Certain professions inherently carry a higher risk of exposure to STDs due to the nature of the job and the potential contact with infectious materials. Obstetricians, gynecologists, and other healthcare providers who are routinely in contact with bodily fluids, may have an increased risk of exposure.
Hospital staff, including nurses and janitors, are also more vulnerable. They handle materials like needles and waste, which could be contaminated.
First responders and aid workers, although trained to handle emergencies, might encounter situations where protective barriers fail or are unavailable, exposing them to a plethora of pathogens. Similarly, adult entertainers and sex workers operate in environments where the risk of contracting and spreading STDs is significantly amplified due to the frequency and nature of their exposure.
Professions that involve frequent close physical contact or exposure to bodily fluids need to be astutely conscious of the associated risks. Adherence to strict hygiene and protective protocols is paramount to minimize the jeopardy of infection. In such fields, the importance of regular STD testing can’t be overstressed, as can the need to stay informed about the latest prevention and safety techniques. Careful vigilance can make a world of difference in these high-risk professions.
Normal Anomalies: Ingrown Hairs and UTIs
Ingrown hairs and urinary tract infections (UTIs) can present symptoms similar to certain STDs, but are commonly occurring and typically non-sexually transmitted conditions.
- Ingrown Hairs: Small, raised bumps resembling pimples, possibly with pus or blood; may cause discomfort or itchiness.
- UTIs: Characterized by a burning sensation during urination, frequent urges to urinate, and cloudy or strong-smelling urine.Both conditions are usually treatable and should be distinguished from more serious STD symptoms through medical evaluation.
While ingrown hairs often resolve on their own, UTIs require medical intervention and antibiotic treatment to prevent complications.
Silent STDs: When There Are No Clear Indicators
Many STDs can exist covertly, offering no overt signs to the infected individual or their partners.
- Human Papillomavirus (HPV): Often asymptomatic, but can lead to genital warts or cancer.
- Chlamydia: Typically silent, yet it can cause serious reproductive damage if untreated.
- Gonorrhea: May exhibit no symptoms, particularly in women.
- Hepatitis B: Largely asymptomatic in early stages; can progress to liver disease.
- Syphilis: Can proceed through stages, initially causing few or no symptoms.
- Herpes (HSV-1 and HSV-2): Many do not have noticeable outbreaks or symptoms.
- HIV: Early infection often mimics the flu or goes unnoticed, later affecting the immune system.
- Trichomoniasis: Symptoms are often mild or absent but can cause irritation and discharge.Symptom absence does not equate to risk absence; STDs can silently undermine health.
Conclusively, silent STDs underscore the necessity for regular, comprehensive sexual health screenings.
Safe Sex Practices: Reducing Your Risk
Condoms are essential barriers against STDs and unintended pregnancies. These simple devices, when used correctly and consistently, can prevent the transfer of bodily fluids, thereby significantly reducing the likelihood of contracting or transmitting infections. Remember, only latex or polyurethane condoms offer comprehensive protection.
Engage in open dialogue about sexual health before intimacy. Honest conversations about past STD testing, sexual history, and expectations set a foundation for trust and responsible sexual behavior.
Adopting preventive measures is key to ensuring long-term reproductive health. Consequently, adhering to a schedule for comprehensive STD testing, particularly after new or multiple sexual encounters, is prudent.
Medically Reviewed by William Terranova, MD on April 23, 2024
Secure and Confidential
STD testing services
The fastest results possbile - available in 1 to 2 days

Tagged
Categorized As
Author: Kristena Ducre
Kristena is a sex-positive LGBTQ ally and general fan of sexy things. As a writer, she is passionate about empowering people's sex lives with accurate and straightforward information. Sex can be a ton of fun, but sexual health is not a laughing matter. In the bedroom, as in life, knowledge is power.




