Spermatoceles
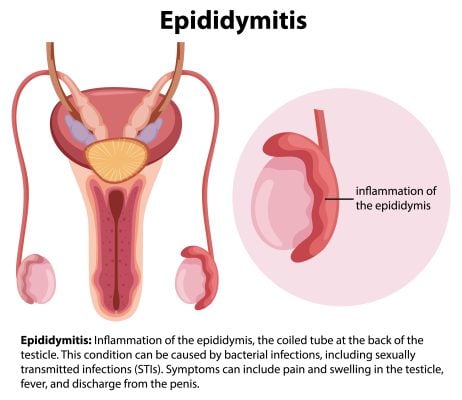
Spermatoceles, also known as spermatic cysts, are benign growths that occur in the epididymis, a small, coiled tube located at the rear of each testicle where sperm is stored and matured. These fluid-filled sacs do not usually cause pain or require treatment unless they become large or uncomfortable.
A spermatocele typically appears as a small, firm lump near the testicle, often mistaken for a testicular tumor. However, unlike a cancerous growth, a spermatocele is generally harmless and does not affect a man’s fertility.
This article provides an exhaustive overview of spermatoceles, including their causes, symptoms, treatment options, and lifestyle implications. Understanding this condition is essential for maintaining male reproductive health and addressing any concerns about sexual well-being.
Understanding Spermatoceles
Spermatoceles, or epididymal cysts, are benign growths that emerge within the epididymis, a duct behind the testes where sperm matures and is stored. They are characterized by their fluid-filled nature, typically containing a milky or clear liquid and, occasionally, sperm.
The formation of spermatoceles has yet to be entirely understood. However, it’s hypothesized that they occur due to a blockage in the tubes transporting sperm away from the testicles. This blockage could result from inflammation, physical trauma, or an abnormal reabsorption process.
Regarding anatomy, the essential structure involved in spermatoceles is the epididymis, which comprises a series of small tubes. These tubes connect the testes to the vas deferens, larger ducts that transport sperm to the urethra for ejaculation. The blockage and subsequent cyst formation primarily occur within the delicate tubing of the epididymis.
While spermatoceles are usually small and cause no symptoms, they can grow larger over time. When they reach a significant size, they might lead to discomfort or a sensation of heaviness in the testicle. Despite these potential symptoms, it’s important to note that spermatoceles do not typically affect fertility or sexual function.
Spermatocele Symptoms and Diagnosis
As mentioned, most spermatoceles are asymptomatic, meaning they do not cause noticeable symptoms. They are often discovered during a physical examination or self-examination of the testicles for other conditions. However, when symptoms do occur, they might include:
- A feeling of heaviness in the testicle with the spermatocele.
- A lump or swelling behind or above the testicle.
- Discomfort or mild pain in the affected testicle.
See a doctor if you discover any lumps in your testicles or if you experience discomfort or swelling in the scrotum. While most lumps are not cancerous, ruling out severe conditions like testicular cancer is crucial.
Diagnostic Procedures
The primary method of diagnosing a spermatocele is through a physical examination. The doctor may shine a light behind the testicles (transillumination) to check if the cyst is filled with solid fluid. If the exam is inconclusive, the doctor may order an ultrasound. An ultrasound can distinguish a spermatocele from other conditions, such as a hydrocele (fluid-filled sac around a testicle) or a varicocele (enlarged veins in the scrotum). Further tests may be needed to rule out testicular cancer in some cases. These could include blood tests to look for tumor markers or, in rare instances, a biopsy.

Causes of Spermatoceles
The exact cause of spermatoceles remains somewhat of a mystery to medical professionals. However, they are believed to result from a blockage in the tubes that transport sperm. This obstruction could lead to a buildup of sperm that eventually forms into a cyst.
While the specific cause is unclear, several factors may increase the risk of developing a spermatocele:
- Age: Spermatoceles can occur at any age but are most common in men aged 20 to 50.
- Previous surgery: Men who have had surgery on their scrotum, mainly if it involved the epididymis or the vas deferens, may be at a higher risk.
- Trauma or inflammation: Any injury to the scrotum or an inflammatory condition can increase the risk of spermatocele.
- Genetic predisposition: There seems to be some indication that spermatoceles may run in families, although more research is needed.
It’s important to note that having a risk factor does not mean you will develop the condition. Many men with one or more risk factors never develop a spermatocele, while others with no known risk factors do. Comprehending these risk factors can help in early detection and prevention strategies.
Spermatocele Treatment Options
Spermatoceles typically don’t require treatment unless they cause significant discomfort or pain. When treatment is necessary, the options range from conservative measures to surgical intervention.
Conservative Measures
Observation is often the first action, especially for smaller, asymptomatic spermatoceles. Regular check-ups will be scheduled to monitor any changes in size or symptoms.
Pain management is another conservative approach. Over-the-counter pain medicines, like acetaminophen or ibuprofen, may be recommended by your doc to alleviate discomfort.
Wearing an athletic supporter can support the scrotum and help reduce pain or aches caused by a large spermatocele.
Spermatocele Surgical Options
If a spermatocele causes significant symptoms or continues to grow, surgery might be required. The standard procedure is a spermatocelectomy, where the surgeon incisions the scrotum and removes the spermatocele.
Another option is aspiration with sclerotherapy. In this procedure, the fluid inside the spermatocele is drained with a needle. Then, a chemical is injected into the sac to cause scarring and prevent the spermatocele from refilling with fluid. This method is less invasive but has a higher recurrence rate than spermatocelectomy.

Spermatocelectomy
Spermatocelectomy is a surgical procedure to remove spermatoceles that cause discomfort or other symptoms. Spermatoceles, also known as epididymal cysts, are benign, fluid-filled growths in the epididymis, a small organ attached to the testicle.
The procedure is generally performed outpatient, using either local or general anesthesia. During the surgery, the surgeon incurs the scrotum and removes the spermatocele.
Spermatocele Post-Treatment Care
Post-treatment care will depend on the chosen treatment option. Keeping the incision area clean and dry is crucial for surgical procedures to prevent infection. Pain meds may be prescribed to manage pain after surgery.
Regular follow-up visits will be necessary for surgical and non-surgical treatments to monitor recovery and ensure the spermatocele has not returned.
Is Spermatoceles a Sexually Transmitted Disease (STD)?
Spermatoceles are not sexually transmitted diseases (STDs), and it’s crucial to clear up this common misconception. They are benign cysts that form in the epididymis, a small organ located at the back of the testicle that holds and ferries sperm. Spermatoceles are not caused by sexual activity and cannot be passed on to a partner.
Differences between Spermatoceles and STDs
While spermatoceles and some STDs may cause a lump or swelling in the scrotum, the similarities end there. STDs are infections passed from one person to another via sexual contact, including intercourse, oral sex, and anal sex. Bacteria, viruses, or parasites cause them. On the other hand, spermatoceles are believed to result from a blockage in the tubes that transport sperm, leading to a buildup of sperm that forms into a cyst.
Explanation of How Spermatoceles is Not Contagious
Unlike STDs, spermatoceles are not infectious or contagious. They cannot be spread to a sexual partner through contact, bodily fluids, or sexual activity. A spermatocele does not impact a person’s sexual health or fertility. However, if a spermatocele causes discomfort during sexual activities, it may indirectly affect a person’s sexual life.
Frequently Asked Questions about Spermatoceles
1. Can a spermatocele affect fertility?
Spermatoceles generally do not affect a man’s fertility. They are benign and typically don’t interfere with the function of the testicles or the epididymis.
2. Can a spermatocele go away on its own?
In some cases, small spermatoceles may shrink or even disappear over time without treatment. However, larger ones tend to remain the same size or grow and may require medical intervention.
3. Is the surgery for a spermatocele risky?
As with any surgery, there are risks associated with spermatocelectomy, such as infection, bleeding, and damage to surrounding tissues. However, it’s generally considered a safe procedure by an experienced surgeon.
4. How long is the recovery after a spermatocelectomy?
Recovery times vary depending on the individual’s overall health and the size of the spermatocele removed. Most men can return to light activity within a few days, but strenuous or sexual activity should be avoided for a few weeks.
5. Can a spermatocele come back after treatment?
Although rare, a spermatocele can recur after treatment, particularly after aspiration and sclerotherapy. Regular follow-up visits with your doctor can assist in detecting any recurrence early.
Living with Spermatoceles
Living with spermatoceles can be relatively straightforward, as many cases are asymptomatic and don’t interfere with daily life. However, for those experiencing discomfort or emotional distress, certain lifestyle modifications, coping mechanisms, and support networks can be beneficial.
Lifestyle Modifications
For those experiencing discomfort due to a larger spermatocele, certain lifestyle modifications can help manage symptoms. Wearing supportive underwear like briefs or athletic supporters can help reduce discomfort by providing extra support to the scrotum. Over-the-counter pain relievers can also be used to manage mild discomfort. Avoiding activities that exacerbate discomfort, such as heavy lifting or intense physical activity, can also be beneficial.
Coping Mechanisms
Living with a spermatocele can cause anxiety or distress for some men, mainly if the cyst is large or causes discomfort. Cognitive-behavioral therapy (CBT) can help manage these feelings. CBT is a form of treatment that allows individuals to transform harmful thought patterns and behaviors.
Mindfulness and relaxation techniques like breathing or yoga can reduce stress and improve overall well-being.
Support Networks
Support networks play a crucial role in coping with any health condition. Reach out to friends and family for emotional support. Joining a support group in person or online can also be beneficial. Support groups supply a secure place to share experiences, learn from others going through the same situation, and receive encouragement and understanding.
Conclusion
Spermatoceles, or epididymal cysts, are benign and typically harmless growths in the epididymis, a small organ located at the back of the testicle. They are not sexually transmitted diseases and are not contagious.
While most spermatoceles do not cause symptoms, larger ones can cause discomfort or a feeling of heaviness or pain in the testicle. However, they generally do not affect a man’s fertility or sexual health. If a spermatocele causes significant discomfort, treatment options such as aspiration, sclerotherapy, or surgical removal are available.
Living with a spermatocele requires little to no lifestyle modifications for most men. Still, those experiencing discomfort or distress may benefit from supportive measures like wearing supportive underwear, adopting stress-reducing activities, and joining support networks.
Regular follow-ups with a healthcare provider are essential to monitor the condition and ensure appropriate care. As with any health concern, early detection and proper treatment are vital to managing spermatoceles effectively.
Medically Reviewed by William Terranova, MD on September 25, 2023
Secure and Confidential
STD testing services
The fastest results possbile - available in 1 to 2 days

Tagged
Categorized As
Author: STD Check Editorial Team
At STDCheck.com, we go to great lengths to ensure quality content. We’re using our own collection of data. It is not bought or made up for “click-bait” purposes. We don’t entice traffic with cheesy graphics or raunchy headlines. Our information is to promote STD testing, educate people, let go of social stigmas, and bring awareness. We also provide a completely confidential atmosphere through private testing. When we produce an article, it is fact-based. We check it with medical advisors that approve it. Our staff consists of doctors and other medical professionals who peer review the content we make available on STDCheck.com. From all over the world, we have sourced the best and the brightest content developers, including medical professionals, marketing engineers, data scientists, content specialists, and media relations.