Understanding Parasitic STDs: What You Need to Know
Have you ever considered what unseen threats could disrupt your intimate health? Imagine an invader, not much larger than a speck of dust, wreaking havoc on your well-being.
Now, picture that nanoscopic menace as a sexually transmitted parasite, a stealthy catalyst for discomfort and distress – these are the realities of parasitic STDs looming in intimate encounters.
Identifying Parasitic STDs
To recognize the signs of parasitic STDs, awareness of their distinct symptoms is crucial. Trichomoniasis may present with genital discomfort and unusual discharge, while scabies induces severe itching due to the mites burrowing into the skin. Pubic lice, or “crabs,” lead to intense itchiness and visible nits on the hair of the affected area. It is imperative to observe these signs meticulously, as early detection can significantly aid in managing these conditions.
Proper diagnosis of these parasitic infections hinges on clinical assessment and laboratory testing. If you notice persistent itching, changes in genital discharge, or any other unusual symptoms, it is advisable to seek professional medical evaluation. Timely intervention not only remedies your discomfort but also prevents the potential spread of these insidious infections to others.
Recognizing Trichomoniasis
Trichomoniasis often presents discreetly, the absence of symptoms obscuring the infection’s propagation among sexually active individuals.
Trichomoniasis disproportionately affects women, casting a spotlight on the need for routine screening in female populations.
Characteristic symptoms of trichomoniasis include genital itching, abnormal discharge, and discomfort during urination, all suggestive of the parasitic invasion.
Despite its stealthy nature, diagnosis is readily achieved through specific tests, putting the invisible adversary of trichomoniasis firmly within the scope of medical intervention.
Signs of Scabies Infection
A telltale sign of a scabies infection is intense itching, particularly at night, which stems from an allergic reaction to the mites. Small blisters or pimple-like bumps may appear on the skin.
Burrow tracks made by female mites can be discernible as irregular, thread-like lines on the skin’s surface.
The rash associated with scabies often involves the wrists, between the fingers, armpits, and the genital area.
Symptoms can take four to six weeks to develop after infestation, making early detection challenging without close examination of the skin for mites or their eggs. Severe cases may result in widespread skin rashes and scaling, indicative of a more entrenched infestation requiring immediate treatment.
Detecting Pubic Lice Presence
The identification of Pthirus pubis may be elusive, appearing initially as unassuming skin itchiness around the genital area.
Inspection of the pubic region often reveals tiny, crab-like insects visually or as bluish-gray skin macules resulting from their feeding activity.
Close observation discloses nits, egg casings of these parasites, tenaciously affixed to the base of pubic hairs, signaling infestation. Utilization of a magnifying lens enhances detection capabilities, allowing for the discernment of lice and nits otherwise indistinguishable to the naked eye.
Prompt recognition of these symptoms warrants professional medical consultation, facilitating timely treatment and halting potential transmission.
Transmission Pathways Explored
Parasitic STDs disseminate through intimate physical contact, typically requiring the direct exchange of bodily fluids or skin-to-skin interaction. The strategic positioning of parasites, such as Trichomonas vaginalis, Sarcoptes scabiei, and Pthirus pubis, demands proximity to warm and humid environments, hence their predilection for genital areas. Intimate contact facilitates these parasites’ transmission, exploiting the closeness inherent in sexual activities to propagate and sustain their life cycles.
Understanding these transmission pathways underscores the importance of preventative measures and the necessity of prompt diagnosis and intervention. While non-sexual transmission is possible, via shared clothing, bed linens, or towels, it is substantially less common compared to the sexual route, emphasizing the significance of safe sexual practices in controlling the spread of parasitic STDs.

Sexual and Non-Sexual Spread
Parasitic STDs, including trichomoniasis, scabies, and pubic lice, are primarily transmitted through sexual contact. Engaging in intercourse with an infected partner can swiftly transfer these parasites, making precautionary measures such as condom usage crucial for prevention.
Non-sexual transmission, although less common, is indeed plausible for these parasites. Shared personal items like bedding or clothing can harbor these infestations, leading to their spread.
For instance, scabies mites can survive away from the human body, lingering in fabrics. Contact with such contaminated items can result in transmission, underlining the importance of hygiene.
In the case of pubic lice, sharing towels or undergarments can facilitate the movement of lice from one individual to another. This highlights the need for personal hygiene and caution in communal living spaces to prevent sharing more than amenities.
Despite the dominant sexual transmission route, these parasitic infesters are opportunistic. They will exploit any avenue available, making vigilance in all aspects of personal contact and hygiene indispensable in their containment.

Risks Associated with Common Items
Personal items, especially those in close contact with the body like underwear, can harbor parasitic STDs. Shared or improperly laundered items could potentially become vehicles for the transmission of parasites.
Even common household linens pose a risk. Parasites can linger, waiting for a new host. Bedding, in particular, can retain parasites between uses. Vigilance in laundering at high temperatures (to kill organisms) is therefore essential.
Grooming tools like razors, used on or near intimate areas, present an often-overlooked risk. Sharing these can inadvertently transfer parasitic STDs even in non-sexual contexts.
Public amenities such as gym equipment, with high contact and turnover rates, may also be a point of concern. Regular cleaning and personal protective barriers like towels can reduce the potential risk of contact with parasitic STDs.
Lastly, attire used in intimate settings, like lingerie, merits careful handling. Washing after each use prevents potential transmission of resilient parasitic agents.
Diagnostic Procedures
To diagnose parasitic STDs, a healthcare provider will conduct a thorough clinical evaluation, including a detailed patient history and physical examination. This initial assessment often guides subsequent diagnostic steps.
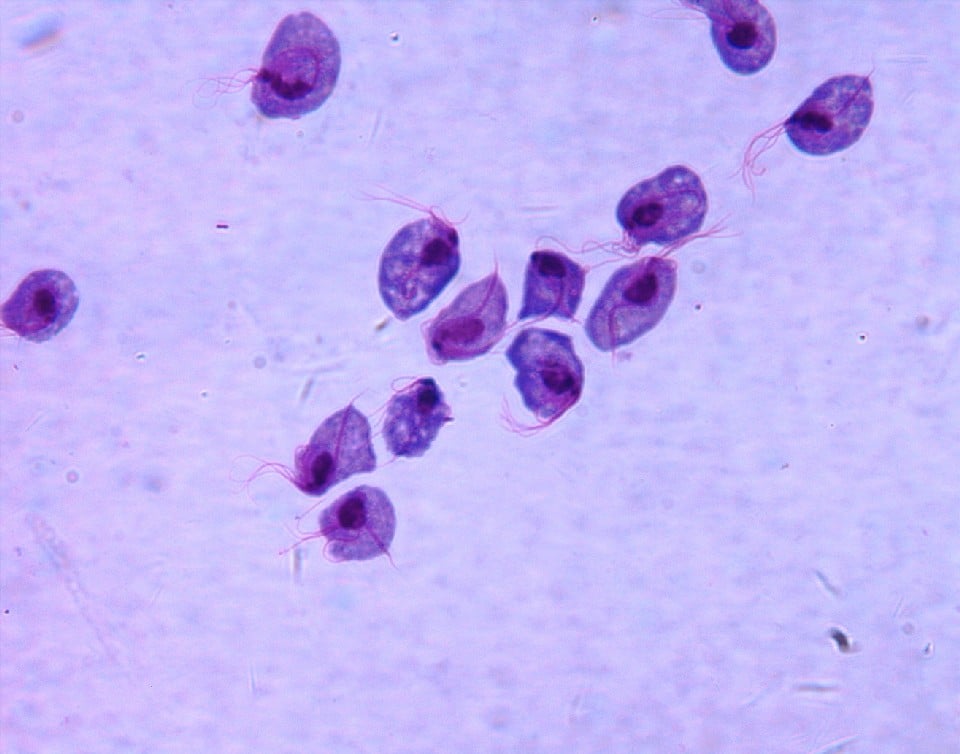
For Trichomoniasis, a microscopic examination of a sample from the genital area — a diagnostic method termed “wet mount” — is a common practice. In cases where scabies or pubic lice are suspected, visual identification of the parasite or their eggs using magnification aids in diagnosis.
Polymerase chain reaction (PCR) tests and culture methods can further corroborate the presence of parasitic infections, ensuring accurate identification and treatment.
Testing for Trichomoniasis
To ascertain the presence of Trichomonas vaginalis, healthcare professionals utilize specific diagnostic tests. These tests are crucial for detecting the infection, especially in asymptomatic individuals.
A nucleic acid amplification test (NAAT) offers high sensitivity for trichomoniasis screening. It amplifies the parasite’s genetic material for easier detection.
For a definitive diagnosis, sampling of urogenital secretions is examined under a microscope. This test, known as a wet mount, can reveal the motile trichomonads indicative of infection.
In the context of treatment efficacy, follow-up examinations play a vital role. Ensuring the complete eradication of Trichomonas vaginalis is fundamental for patient well-being. Men and women previously diagnosed should undergo retesting, ideally three months after treatment, to exclude possible reinfection. Compliance with these protocols maximizes therapeutical success and hinders the further spread of this common parasitic STD.
Identifying Scabies and Pubic Lice
Scabies and pubic lice present distinct symptoms and require meticulous examination for proper identification.
- Intense itching, particularly at night, signifies a potential scabies infestation due to the mite Sarcoptes scabiei burrowing under the skin.
- The appearance of a rash of small red bumps or blisters primarily between the fingers, wrists, waist, and genital areas is characteristic of scabies.
- In contrast, pubic lice manifest through visible nits or lice on pubic hair, accompanied by a gray-blue skin hue in the affected region.
- Genital sores may develop as a result of lice bites or the resultant scratching, signaling the presence of pubic lice.Microscopic examination is often employed to definitively diagnose scabies.
Pubic lice, however, are typically visible to the naked eye, facilitating their identification.
Effective Treatment Strategies
Effective treatment strategies for parasitic STDs necessitate both pharmacological interventions and behavioral modifications. Timely administration of appropriate medication, such as metronidazole or tinidazole for trichomoniasis and permethrin or ivermectin for scabies, is critical for eradicating the infection. Concurrently, patients must adhere strictly to treatment protocols, avoid sexual contact until treatment is complete, and notify recent partners for testing and treatment to prevent re-infection and curb transmission.
Implementing thorough sanitation practices is imperative in the management of parasitic STDs, particularly for pubic lice. Sanitizing clothing, bedding, and personal items exposed to the parasites ensures the comprehensive elimination of the infestation and lessens the likelihood of recurrent outbreaks. Regular screening and prompt treatment of sexual partners are equally vital to the success of these strategies.
Medications for Parasitic STDs
Antiparasitic agents such as metronidazole are prescribed for trichomoniasis, targeting Trichomonas vaginalis with notable efficacy. To maximize treatment success, physician-guided adherence to medication dosage and schedule is paramount, reducing the risk of persistent or recurrent infections.
Permethrin cream stands as the first-line remedy for scabies. This topical application eradicates mites by disrupting their nervous system, effectively halting reproduction and spread.
Oral ivermectin is an alternative option, particularly for crusted scabies. Administered in tablet form, it offers a systemic approach to mite elimination, complementing topical treatments.
Pubic lice infestations necessitate pediculicides, with pyrethrins or permethrin lotion routinely employed. These agents act swiftly to extinguish adult lice, nymphs, and nits, restoring afflicted individuals to a state of comfort and lice-free existence.
Partner treatment is essential in the battle against parasitic STDs. Coordinated, simultaneous treatment of both partners ensures comprehensive management of the infestation, preventing the cyclical nature of re-infection and ensuring the efficacy of therapeutic interventions.
Preventing Re-infection
To prevent the recurrence of parasitic STDs, adherence to prescribed treatment protocols is crucial.
- Instruct all sexual partners to undergo testing and treatment to stop cycles of infection.
- Abstain from sexual contact until treatment completion and confirmation of eradication.
- Wash bedding, clothing, and towels in hot water to eliminate any residual parasites.
- Disinfect or replace personal items that may have come into contact with the infection.
It is paramount to complete the full course of medication, even if symptoms resolve earlier.
Continuous surveillance of your health and routine testing can prevent the stealthy recurrence of these infections.
Medically Reviewed by Julie Hutchinson, MD on April 24, 2024
Secure and Confidential
STD testing services
The fastest results possbile - available in 1 to 2 days

Tagged
Categorized As
Author: Nick Corlis
Nick Corlis is a writer, marketer, and designer. He graduated from Texas State University in San Marcos, Texas, with a degree in Digital Communications. Nick is proud to be able to help eliminate the stigma of STD testing through his writing and is always trying to advocate the importance of your sexual health. Before STDcheck, his favorite way to develop his writing skills was by accepting various writing jobs in college and maintaining multiple blogs. Nick wears many hats here at STDcheck, but specifically enjoys writing accurate, well-researched content that is not only informative and relatable but sometimes also contains memes. When not writing, Nick likes to race cars and go-karts, eat Japanese food, and play games on his computer.




